POTS Awareness in 2024: New Understandings and Treatment Approaches
Written by Melissa Schenkman, MPH, MSJ
Do you know someone who has POTS? Chances are you do.
Newly diagnosed cases of Postural Orthostatic Tachycardia Syndrome, aka POTS, have been on the rise as one of the post-infectious syndromes people, many under age 50, have developed in the aftermath of COVID-19 Pandemic.
In fact, before the pandemic, an estimated 1-3 million Americans had POTS. According to Dysautonomia International, that number has doubled since COVID-19.
While POTS is far from old (the term was officially coined by researchers at the Mayo Clinic in 1993), its surge in recognition is new and thankfully growing.
POTS is a form of dysautonomia—a disorder of the autonomic system—a highway of nerves throughout your body that actively and automatically—at all times—controls our heartbeat, breathing, blood flow, and other functions.
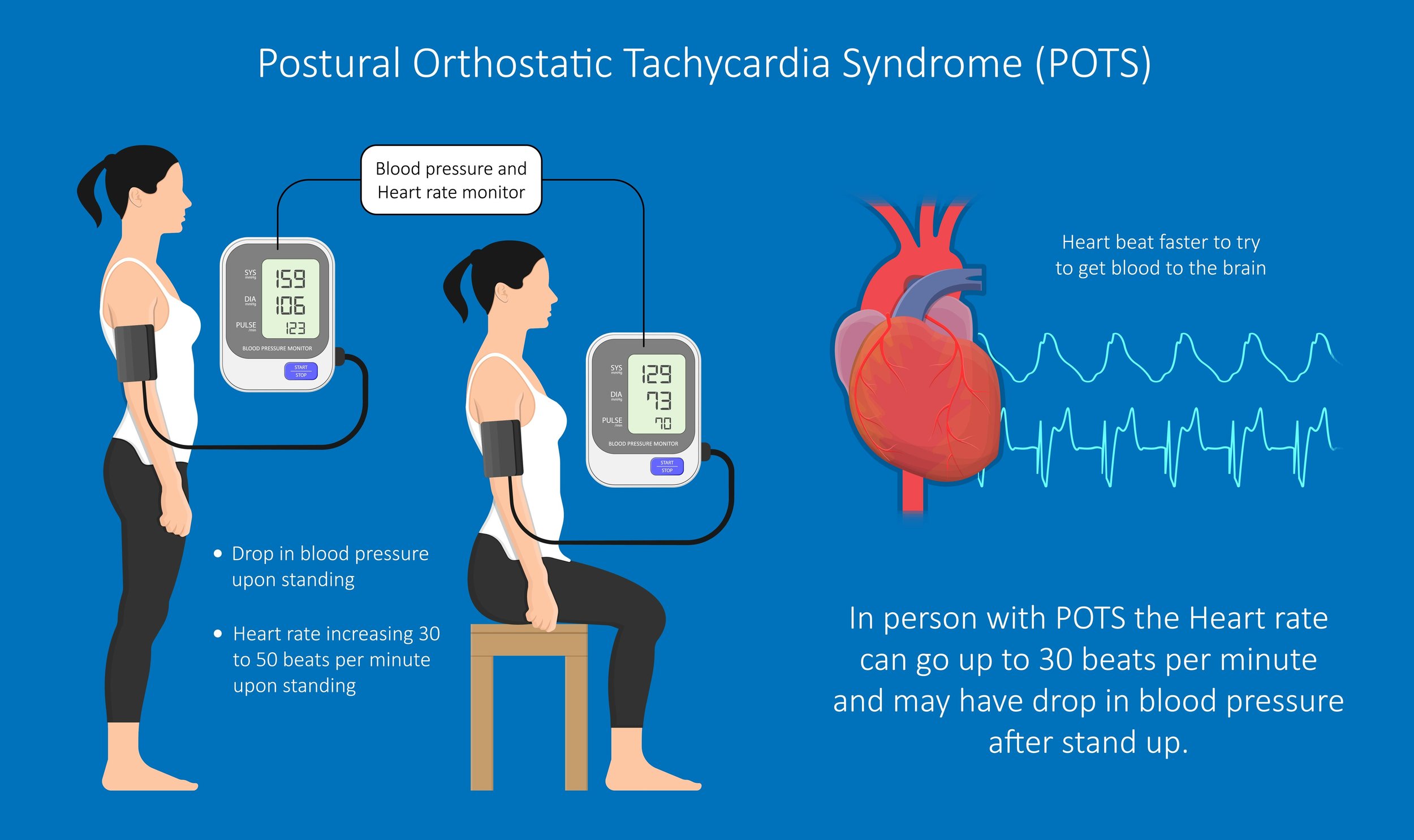
In POTS, the body’s blood flow becomes dysregulated, so that when a person stands upright blood pools in the legs and not enough blood is pumped back up to the brain and heart. This leads to lightheadedness sometimes with fainting, heart palpitations, tremors, nausea, and other symptoms. Currently there is no cure.
The variety of symptoms and the fact that every patient presents so differently can make diagnosing POTS and finding proper treatment for it exceedingly difficult.
That’s something Dr. Sarah Diekman knows firsthand. She has lived with POTS her entire life and is one of the few physicians in the country who specializes in treating patients with the condition in her practice, Diekman Dysautonomia LLC.
As a trained researcher in epidemiology and biostatistics, she shares her insights with us on recent and exciting developments in POTS research—treatment options, the pathways to its underlying causes, and the connection with other conditions, like Long COVID. Diekman also empowers us with how to recognize POTS symptoms and what the future of POTS treatments holds.
Evolving POTS diagnosis approaches
While the traditional method of POTS diagnosis, the Tilt table test, is still the standard, the accepted diagnostic criteria has expanded to include bedside orthostatic vitals.
“This is the ‘poor man's tilt table,’ so to speak, which is much more accessible. It’s kind of the rule of thumb that if the bedside or the orthostatic vitals are positive, then you don't need the tilt table test because what the tilt table test is doing is taking the muscle tone out of the equation,” Diekman explained.
“The muscle in the leg can help compensate for some of the circulation failures that are happening. So, if somebody is positive, even with their muscle tone engaged, they're almost certainly going to be positive on a tilt table. It's very rare that they wouldn't be.”
To note, orthostatic blood pressure readings refer to taking a person’s blood pressure in three different positions: sitting, lying down, and standing, and comparing them.
The only time Diekman has seen the test be positive with muscle tone engaged is when a tilt table was incorrectly executed.
“You're supposed to be in a really calm room without stimulus going on, in part to get the resting heart rate to be as low as possible because you're looking for, at least in an adult, 30 beats per minute difference between when a person is lying and tilted. So, if someone isn't fully at a low resting heart rate, then you may not see that 30 beats per minute difference,” she further explained.
Diekman shared that what is really needed as a tool for diagnosing POTS is accessible cerebral blood flow measurements. These assess how much blood is flowing to the brain. Right now, only a few practitioners, mostly in research settings, are able to do that, she told us.
“I suggest that patients go on a tilt table even though they have the positive poor man's tilt table. It just gives them that more bulletproof evidence, frankly, because sometimes people are in fights against powers that don't have their best interests involved. So, I try to get as much objective evidence. I always try to get as precise of the diagnosis as possible, because even though it may not clinically make a difference right now, who knows what's just around the bend,” she said.
Sarah Diekman, MD, JD, MS, MPH, is a Postural Orthostatic Tachycardia Syndrome (POTS) and Dysautonomia expert who is board-certified Preventive Medicine physician.
Diekman earned her MD and her MS in Biology/Biological Sciences from Indiana University.
She then went on to pursue and earn her JD at Florida Agricultural and Mechanical University. She did her residency in Occupational and Environmental Medicine at Johns Hopkins University, where she was Chief Resident. She earned her MPH at the John Hopkins Bloomberg School of Public Health.
Emerging POTS treatment options
Low-dose Naltrexone: A new player in POTS management
You likely have heard of naltrexone—the drug used to reverse opioid overdoses. It’s an opioid receptor blocker used to treat opioid use disorder. When used in this case the dose is 50 milligrams, but when used at a low dose like .5 to 5 milligrams, the pharmacology is actually very different.
“It has minimal effects on the actual opioid receptors to the point where some people who are on opioids for pain can still take it. Not everyone can tolerate it, but some people still can, and they still get the analgesic effects of their opioids,” Diekman explained. “At low doses it actually works on a cellular basis decreasing inflammatory cascades by acting on what's called the toll-like receptors and glial cells, which ‘glial’ means glue. They support the neurons.”
“Low dose Naltrexone does help a significant number of people with both classic pots and POTS that preceded COVID. But the classic POTS population has benefited from this wave of Long COVID coming in here, because low-dose naltrexone really made it onto the scene for the Long COVID patients.”
The promise of interleukin-6 targeting drugs
It’s long been suspected that an immune system dysfunction underlies of POTS. While the specifics remain a mystery, “all signs are pointing towards interleukin-6 from lots of studies, which are truly cutting-edge bench research” she said.
What is interleukin-6?
It’s a type of cytokine that plays a big role in our immune system. A drug targeting its function could potentially reverse immune dysfunction that is contributing to POTS and its symptoms.
“Cytokines are chemical messengers of the body. “They're essentially like the Postal Service, but they're like the letters. So, they're going to different parts of the body, sending the message and bringing the message to that location,” Diekman explained. “I've read multiple papers now pointing to interleukin-6, and that's exciting because the more we know about a problem, the more we have the ability to solve it.”
Non-pharmacological interventions
At baseline, exercise intolerance is part of POTS. So, exercise has been controversial as a non-pharmacological intervention for POTS because it can help or harm the condition, and it completely depends on each person since POTS has multiple causes.
“I know a lot of institutions are working on better protocols,” Diekman shared. “It's easier said than done though.” Since there are different subtypes, each person living with POTS will have a different level of exercise tolerance.
“Exercise really takes one of two paths. Either people need to pace themselves—pacing being for the most severe exercise intolerance. This basically means that exercise is toxic to them, causing harm,” Diekman explained. On the other hand, some people are able progress in their ability to exercise without it causing harm to their POTS.
“For some people, it can make them feel much better, me included. As a clinician, I have to carefully assess with each person how they’re going to tolerate exercise, and then we keep reevaluating if it is helping or hurting,” she said.
As for complementary medicine’s role in POTS, she likes acupuncture if you are getting it done from a licensed acupuncturist and massage from a licensed massage therapist. “Massage being excellent for lymphatic drainage, for muscle and nerve stimulation, and circulation,” Diekman said.
She has also had some patients have good results with biofeedback–an alternative therapy that helps you take control of certain involuntary bodily functions like breathing.
“I recommend in-person biofeedback, where they can actually put the devices often on the ear because the whole point is that they see what's happening in your body and do the feedback with it,” she explained.
Some of her patients have found hypnosis helpful, which she believes can work in disrupting the pattern of the brain constantly reacting in a way as if it is not getting enough blood all the time, even during times that it is.
“These therapies have the potential to help, but they are not going to help when used alone because unless you’re getting enough blood to the brain, nothing’s ever going to help,” Diekman pointed out.
The complex relationship between POTS and other condition
While the science behind POTS continues to emerge, it is clear that the POTS is part of a constellation of other conditions.
POTS has long overlapped with Myalgic Encephalomyelitis, a condition also known as Chronic Fatigue Syndrome but what led to the two conditions diverging is unknown.
People with POTS tend to also have the connective tissue disorder, Ehlers-Danlos syndrome, but the exact relationship between the two is not known. Recently, exciting research showed that fibrin–a major player in our blood clotting cascade–can trigger an immune response, which may explain the relationship between these two given the role of blood and the immune system.
Additionally, fibrin is a part of actual connective tissue, which is what is affected in Ehlers-Danlos syndrome. As a result, people have fragile skin, so they bruise and bleed more easily (a process fibrin is also involved in).
In the aftermath of the COVID-19 pandemic, a connection between POTS and Long COVID has been identified, although the relationship is still not fully understood. In some cases, Long COVID is actually presenting as POTS.
Patient empowerment and self-advocacy
You have to be your own health advocate. Where that starts with is recognizing the symptoms that you are experiencing are because you have POTS or another post-viral illness because for busy, on-the-go millennials we can attribute them to our hectic lifestyles.
“That's how you're suffering from unexplained fatigue, unexplained brain fog. You can't stand up as long as you used to. You're stuck in bed all the time, having stomach problems that are going on all the time. Can't explain getting rashes, can't tolerate the heat. These can all be signs of either Long COVID, POTS, or a general dysautonomia,” Diekman explained, and we must watch out for them and be aware.
She also encourages you as part of your self-advocacy to do a Google search of these symptoms, if you are experiencing them.
“I know a lot of my colleagues hate when patients go on Google, but that’s too bad. A Google search on these symptoms that are often misdiagnosed will give you an idea of what your illness is,” Diekman. This knowledge can be incredibly helpful in conversations with your healthcare physicians and as you navigate our complex system.
Although, we encourage you to choose reliable health resources on Google to get your information from. You can find a list at the bottom of this article.
The road ahead
As we look to the future of POTS diagnosis and treatment, there’s no doubt that the road ahead is shining more brightly than it has ever been. A few things to keep in mind:
Right now, most treatments for POTS are off-label, generic medications. There are still challenges in treatment accessibility and affordability for more targeted treatments.
There is potential for personalized medicine in POTS by using biomarkers, which would make it more compelling for insurance companies to provide coverage of more drugs targeting the underlying mechanisms of the condition. This will be more important as more medications are developed that are capable of actually getting people closer to cures and remission become available, Diekman said.
It’s a very exciting time in POTS research, with new evidence about underlying mechanisms and potential targets for treatments emerging on a regular basis.
“When I was first diagnosed about 14 years ago, I had absolutely not a scintilla of hope that this disease would be cured in my lifetime. I just focused on symptomatology, like treatment management for myself and then for my patients,” Diekman reflected.
But her outlook has changed. She has even more optimism about what is within our reach, and she wants you to be as well.
“In the last three years now, I really think that a cure is on the table with the amount of money that is going into Long COVID, which is essentially a type of dysautonomia for most people, and very similar to POTS.”
Subscribe to the YMyHealth newsletter to stay up to date on everything that’s health-related for millennials!