Living with Rheumatoid Arthritis in Your 20s, 30s, and 40s
Written by Melissa Schenkman, MPH, MSJ
What do you know about Rheumatoid Arthritis?
You have likely heard the name, maybe even that it’s a type of autoimmune disease, but beyond that for many in Generation Y and Z it’s likely that it’s still a bit of mystery to you as to what it can do to the body and how it can affect a person’s daily life.
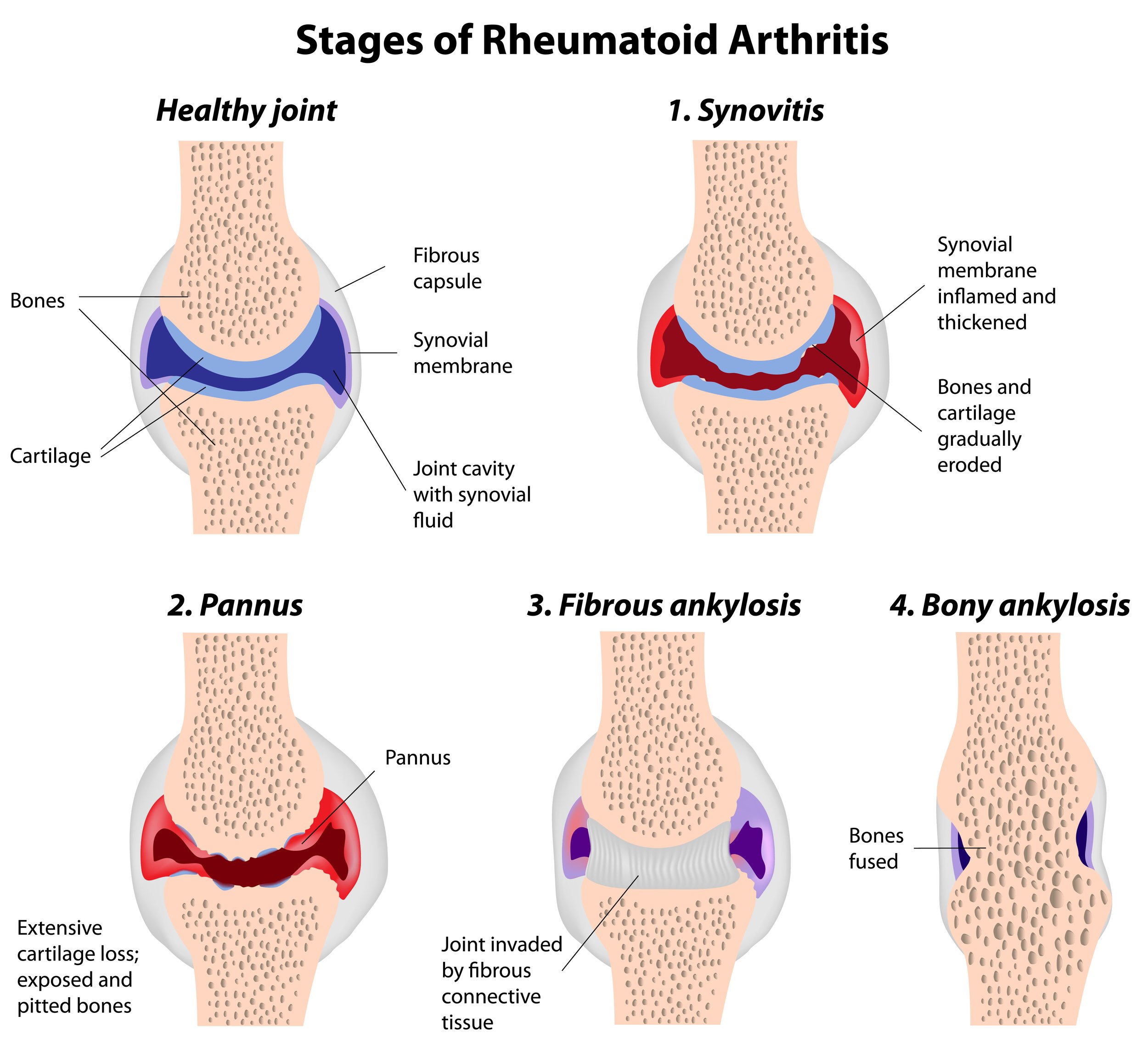
Yes, Rheumatoid Arthritis (RA) is an autoimmune disease, which means the body’s immune system attacks its own tissues. In RA these attacks mainly target the tissue lining your joints. This causes pain and swelling and can lead to potential deformities.
But did you also know it’s a condition that is often diagnosed in your 30s and 40s, meaning it can be developing throughout the millennial age spectrum and even as early as in Gen Z, with the oldest member of that generation now at age 27?
Given our busy lifestyles and the way symptoms appear, we can easily brush them off and think they are caused by just ‘doing too much’ in our daily lives. Especially for females—who are three times more likely to be diagnosed with RA compared to men.
Diana Girnita, MD, PhD, FACR, who is a leading rheumatologist and the Founder Rheumatologist OnCall, breaks down the complexities of RA symptoms, its presentation, and the role of genetics.
She shares how RA can impact daily life, strategies to manage it, long-term health considerations, and treatments on the horizon as a result of cutting-edge research.
Diagnosis and Presentation
It can take months to years to receive a proper diagnosis of Rheumatoid Arthritis.
This is due to the fact that there are so many more patients than rheumatologists in the US. Girnita estimates that there are 1.5 million with RA.
If you live in a large metropolitan area, you will likely have faster and greater access to a rheumatologist than someone who lives in a rural area. For those patients, the nearest rheumatologist can be hundreds or even thousands of miles away.
Another determining factor is pain tolerance during the early stages of Rheumatoid Arthritis.
“Remember, a lot of females tolerate a lot of pain. They want to be tough and brush it off, thinking ‘Maybe I did too much,” Girnita said. “There are so many activities that you do with your hands that will cause joint pain, but joint pain in young females is not what you should normally expect.”
The early signs of Rheumatoid Arthritis primarily involve joint pain in the hand, especially in the small joints and wrist.
“It's always symmetric and bilateral [on both sides of the body],” Girnita said. “So, if you have both hands, both wrists, both elbows or shoulders, knees, or both feet in a pattern, you should always think about rheumatoid arthritis. That's very common.”
For females in their 20s, 30s, and 40s, they can often think they have carpal tunnel syndrome from overuse of their wrists in typing on the computer.
But in fact, Girnita assures us that having carpal tunnel syndrome in both wrists is not something commonly experienced in multiple conditions. It only happens in a few types of diseases, RA being one of them.
Other common presentations are extreme fatigue and dryness of the eyes and mouth.
“They start feeling very, very, very tired to the level that will impact their life. And because of that, and joint pain, they will come to be evaluated,” she explained. “The dry eyes and mouth are because of this systemic inflammation that is happening in Rheumatoid Arthritis that will affect the lacrimal glands and the salivary glands,” Girnita shared.
This can lead to what’s known as a secondary form of Sjögren’s Syndrome—another complex autoimmune disorder, but one affecting the glands responsible for producing tears (lacrimal glands) and saliva (salivary glands).
Genetic Factors and Risk
While having close relatives with any type of autoimmune disease can increase your risk, RA is not a genetically transmitted disease, Girnita clarified.
This means that if your mom has RA, she is not going to directly pass it to you for sure. Instead, your risk of developing RA increases when you have a relative who has it.
For example, if you have a first-degree relative (mom, dad, sister, brother) who has RA, you have a three times higher chance of developing it. With a second-degree relative (aunt, uncle, grandparent) who has RA your risk is about twice as high.
“So, there is a genetic predisposition like in many of our autoimmune diseases, but it’s not necessarily that if you have it you are going to pass it to your children for sure,” Girnita said.
Impact on Daily Life
There is no question that being diagnosed with any autoimmune disease is going to impact you for life because it is a chronic condition.
When people are first diagnosed with RA, it causes them a lot of stress, especially for females, who typically already carry so much on their plates. Anxiety and depression are very common.
“At first, a lot of people think that autoimmune disease is a sentence to death, but it is not. We have a lot of options today to treat RA and put it into remission,” Girnita said. “Understanding that you have the power to modulate this disease with the help of a physician and with the help of medication, things will be better.”
The beginning can be particularly hard as doctors try to determine the right treatment approach based on how your symptoms respond to different treatments. This can take four to six months, she told us.
“The more you are in communication with your physician, the more you invest in your lifestyle in combination with the proper medication, the better you are going to be,” Girnita said.
She also recommends people give themselves more grace, especially taking breaks to recover during flare-ups.
“Invest in your well-being, not only mentally but also physically. What the patient does and how the patient thinks is 10 times more important than a medication itself,” Girnita emphasized.
Diana Girnita, MD, PhD, FACR, is the Founder of Rheumatologist OnCall®, a speaker, and author. She is double board-certified in rheumatology and internal medicine. She earned her MD and a PhD in immunology at Universitatea de Medicină și Farmacie din Craiova in Romania, where she grew up. She came to the United States as a PhD student and postdoctoral fellow at Harvard University.
The following year she accepted a postdoctoral research position at the world-famous University of Pittsburgh’s Starzl Transplantation Institute, home of the world’s first liver transplant.
After missing working with patients, she resumed her clinical training, first completing an internal medicine residency and then graduating from the University of Cincinnati’s rheumatology fellowship program.
Managing RA
One of the most important things younger patients and really all patients can do for RA is to exercise. It may seem counterintuitive that you would want to use your joints when that’s one of the primary areas the disease effects, but it’s very beneficial.
Girnita shared that almost any type of exercise that is enjoyable is good for RA from stretching and yoga, to walking and even swimming in the pool.
“The more you move, as awkward as this could be, the better you are going to feel and the flexibility of your joints will be,” Girnita said. “Do not overdo it though.”
Also, the earlier a patient starts treatment, the better. Thankfully, there is so much known about the disease today and many treatment options that can make for a great quality of life.
“That is why it's a pity not to take care of yourself and give medication and lifestyle interventions a try to stop the disease from progressing,” she said. “What I say to my patients that are in their 20s and 30s is: If you don't care about how your hands are going to look in 10 years or 20 years. If you don't care about the fact that you are not going to be able to use your hands. Then, you will care if you're not able to see or if you have a heart attack, or if you're not able to breathe.”
Those are valid reasons, she said, to start treatment as early as possible. After all, there is no cure for RA or any autoimmune disease.
“We don't want to fool patients, but we are able to put them in remission, stop disease progression, and make symptoms like the pain, swelling, and stiffness go away,” Girnita explained. “Rheumatoid Arthritis is also a systemic disease, and if you leave it untreated, unfortunately, it may affect your eyes, your lungs, and your heart, and those are vital organs.
“The earlier you have a diagnosis, the earlier you can start treatment; and the earlier you start lifestyle interventions, the better results you are going to have.”
Treatment Options
Most effective treatments
Girnita shared that there is not one specific treatment that she would say is most effective.
“I think there are different medications for different stages and for different patients. You literally have to come up with a personalized approach,” she said.
In recommending a treatment, she takes into consideration how aggressive a patient’s symptoms are, other medical problems that they have, and other factors. She always explains to patients what the treatment options are from least aggressive to most aggressive and helps to coach them through the process.
Potential side effects
Every person is different when it comes to side effects. Although, most people will have at least one side effect from their RA medication. According to the University of California San Francisco, common side effects from RA treatments include:
Cold symptoms
Stomach upset (such a nausea or diarrhea)
Rash
Managing treatment costs
RA drugs are very expensive, but in many cases insurance companies will pay for them. However, there are patients that don't have great insurance, have very high deductibles to meet, or don’t have any health insurance, Girnita told us. She has looked for resources for those patients and recommends the following:
Purchasing medications with cash
Pharmaceutical company-based programs that help with payment, including subsidized programs that certain types of patients qualify for
Programs sponsored by foundations like the National Arthritis Foundation, which run programs providing one or two years of free medication coverage to certain patients.
Long-Term Health Considerations
As a very prevention-focused generation, millennials always want to know what we can do today to live our healthiest lives tomorrow and long term. Girnita shares our deep interest in that and works to “bridge the two worlds of lifestyle prevention with the traditional Western medicine” in her practice.
In fact, she will be coming out with a book dedicated to RA and the importance of incorporating lifestyle measures that will prevent this disease progressing faster and into something that you don't want to have.
Eating a healthy diet, exercising to maintain joint function and mobility, prioritizing sleep, she told us, are where you can find big wins for your health.
“Those lifestyle interventions are extremely important, and there is a lot of scientific value behind them,” Girnita said. “There are studies that prove that eating a certain type of diet, particularly the Mediterranean type, incorporating that as a lifestyle, not as a diet, which means restriction, is very powerful, as certain foods will decrease the amount of inflammation in your body.”
Managing stress is also a crucial for people living with RA in their 20s, 30s, and 40s.
“At this point in your life, you have a lot of stress. You are building a career. You are having a young family, young kids. We as females try to prioritize everybody else besides us. So, it is very important that we prioritize the lifestyle habits.”
People living with RA should also keep an eye out for these related health conditions: lupus, autoimmune thyroiditis and Sjögren’s Syndrome.
Future Outlook
Treatments of the future will be more personalized, easier to use, and focused on making the immune system less reactive.
In the past decade, she pointed out that there was a move away from predominantly injectable medications to pills for treating RA. She believes even more therapies in pill form will appear.
“Then, I think we're going to start seeing more information about immunotherapies, meaning modifying drugs that will impact or modulate our immune system to quiet it down to not to be so reactive,” Girnita said.
CAR T-cell therapy is one of the most widely known, and it is now being studied in autoimmune disease.
“There was actually a study published last year that included patients with Rheumatoid Arthritis and scleroderma. They gave them CAR T-cell therapy, and these patients were in remission for two years. They are still being followed to see if this remission is for a long time or they have to get treatment again,” Girnita said.
“I am very excited to hear about that because I believe that when we understand how our immune system works, we will be able to treat these diseases much, much better.”
Conclusion
If you are living with RA or have a friend or family member who is and any of you are in your 20s, 30s, or 40s, please know there is so much you have in your control to manage this condition and live your best life, enjoying the things you love to do.
Remember these key takeaways from Dr. Girnita:
Stay in close contact with your rheumatologist and let them help coach you on how to manage RA as you go through different phases of your life
Exercise to maintain joint mobility and flexibility
Eat foods that are part of the Mediterranean diet to reduce inflammation
Reduce your stress through meditation, getting sleep, and practicing mindfulness
Give yourself grace when you have RA flareups and take the time to rest
Be your own health advocate!
We encourage you to do each of these things in collaboration with your rheumatologist.
Finally, remember to always be your own health advocate. Here are two excellent resources to visit for more information on RA:
Rheumatologist OnCall blog (Dr. Girnita)
Subscribe to the YMyHealth newsletter to stay up to date on everything that’s health-related for millennials!